 There is a large screen next to the patient which displays the patient’s vital signs, such as heart rate and rhythm, blood pressure and oxygen levels. This can also be monitored via another screen on the outside of the bed space that relays the same information to the critical care team.
There is a large screen next to the patient which displays the patient’s vital signs, such as heart rate and rhythm, blood pressure and oxygen levels. This can also be monitored via another screen on the outside of the bed space that relays the same information to the critical care team.
Monitors may bleep and alarm to alert the nursing staff of any changes during monitoring. The bedside nurse will explain this to you and can support any questions you may have.
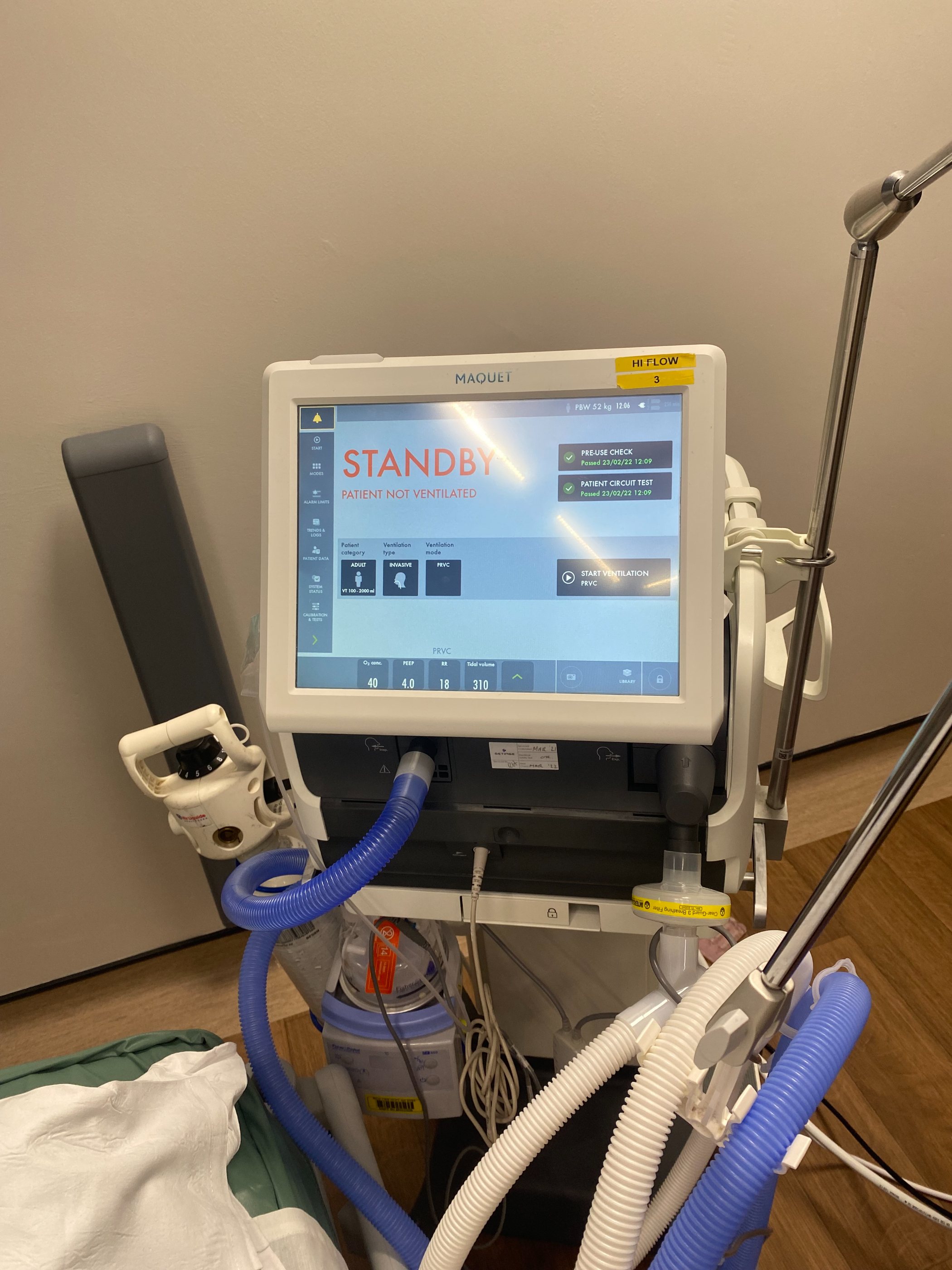 Patients who are not strong enough to breathe on their own and need support will be connected to a ventilator. These are often called life support or breathing machines but are really a device to provide oxygen to a patient that is unable to breathe effectively for themselves.
Patients who are not strong enough to breathe on their own and need support will be connected to a ventilator. These are often called life support or breathing machines but are really a device to provide oxygen to a patient that is unable to breathe effectively for themselves.
To enable this, the patient must first be sedated with medication to allow the passing of a tube called an endotracheal tube into the windpipe via the mouth. This tube is connected to the ventilator which does the work of breathing for the patient. The settings and oxygen requirements can differ during the day so do not be disturbed if changes are required.
The patient will not be able to talk due to the sedation and the endotracheal tube. The medication and sedation will keep the patient comfortable, whilst they are on a ventilator.
Continuous positive airway pressure (CPAP) or Non-Invasive Ventilation (NIV) devices can be used as a step-up from wall oxygen for patients that require greater amounts of oxygen but do not need support from a ventilator. They can be delivered with a tight fitting mask or sometimes via a special hood.
The patient may feel uncomfortable wearing the mask and apparatus, however this should not be painful. It can cause the mouth to feel very dry due to the oxygen being delivered in this way, however the nurse will ensure the patient is able to have a drink and time out of the mask when possible.
If the patient requires a longer period of support with breathing, it may be necessary to perform a tracheostomy. This enables sedation to be reduced and increased interaction with the patient. It can also help reduce the amount of time spent on a ventilator. Although this may appear daunting and strange it is much more comfortable for the patient to wean off the ventilator and nurses can give mouth care more easily.
This involves a procedure to put a tube through the neck into the windpipe allowing the patient to still have support from the breathing machine but also be more awake. This will usually be performed on the critical care unit under the supervision of an intensive care consultant.
Eventually with the aid of a speaking valve, patients will be able to talk to us. If a tracheostomy is felt to be needed, the intensive care consultant will usually discuss this with the patient or family member in advance. A tracheostomy is rarely permanent. Here is more information on the procedure involved.
There may be a need for increased blood testing on critical care in order to closely monitor changes in the patient’s condition and to assess response to therapy.
Artery blood is often tested. This helps us determine blood oxygen levels and look at the acid/base balance of the patient. This may be via an arterial line inserted usually in the wrist or arm; this means we don’t have to use a needle every time to remove blood. We also monitor the blood pressure via this piece of equipment giving us a very accurate reading.
 Patients on critical care often need several different medications including sedation/pain relief, antibiotics and infusions to support the heart and blood pressure. These will be delivered by a number of infusion pumps positioned at the patient bedside.
Patients on critical care often need several different medications including sedation/pain relief, antibiotics and infusions to support the heart and blood pressure. These will be delivered by a number of infusion pumps positioned at the patient bedside.
 A proportion of patients will be admitted to critical care with acute kidney injury or will develop this as a complication of their illness. Some of these will progress to kidney failure and require renal replacement. This machine allows us to support the patient’s kidneys and fluid balance when there is a failure or need to supplement kidney function. This machine performs the role of the kidney and clears away toxins and fluids from the body. It is similar to a dialysis machine.
A proportion of patients will be admitted to critical care with acute kidney injury or will develop this as a complication of their illness. Some of these will progress to kidney failure and require renal replacement. This machine allows us to support the patient’s kidneys and fluid balance when there is a failure or need to supplement kidney function. This machine performs the role of the kidney and clears away toxins and fluids from the body. It is similar to a dialysis machine.
The patient will have a special line inserted in the groin or neck for the machine to take the blood from the patient which will then filtrate and clean it before returning it to the patient.
Most patients only need this procedure whilst in the intensive care unit as a supportive measure during their stay but a small number will need longer term kidney support.

